
Treatments like monoclonal antibody infusions and antiviral pills can prevent a case of COVID from becoming life-threatening. But many of the available drugs are not being utilized.
Emily Elconin/Bloomberg via Getty Images
hide caption
toggle caption
Emily Elconin/Bloomberg via Getty Images
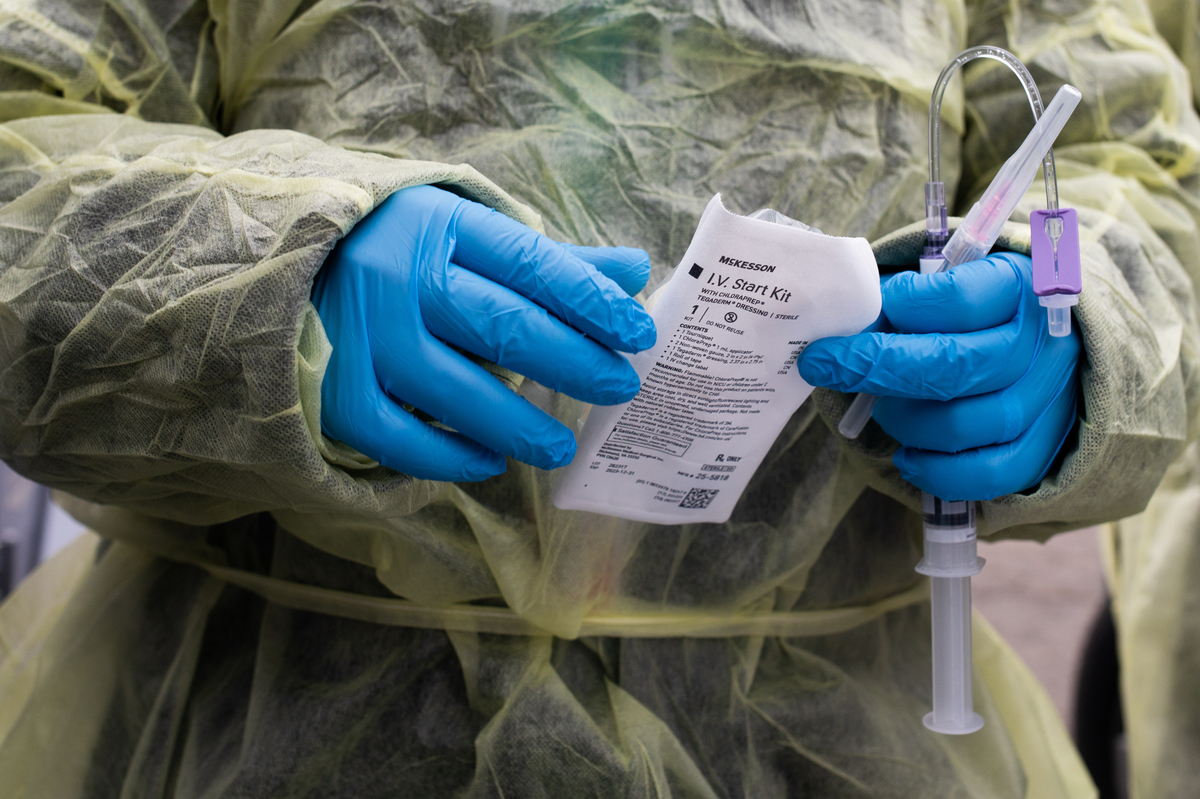
Treatments like monoclonal antibody infusions and antiviral pills can prevent a case of COVID from becoming life-threatening. But many of the available drugs are not being utilized.
Emily Elconin/Bloomberg via Getty Images
Even as this winter’s omicron surge recedes, more than 2,000 people in the U.S. still get hospitalized with COVID-19 each day. This population is largely unvaccinated, with medical conditions that increase their risks. Some of these hospitalizations could have been prevented with early COVID treatments, such as pills and monoclonal antibodies, purchased and distributed for free by the government.
But data on COVID treatment utilization, shared with NPR by the U.S. Department of Health and Human Services, indicates that millions of COVID treatments are sitting on shelves unused.
“We are still in a public health emergency,” said Dr. Derek Eisnor, who leads the government’s distribution of COVID drugs, on a call with national health organizations on March 16. He urged health leaders to try to get the drugs to communities that have a demand for them, rather than let them go to waste.
“There’s an assumption that there’s not enough of [these drugs] around but it does seem when you look at the numbers that there is a lot around — it’s just not being used,” says Dr. Amesh Adalja, an infectious disease physician and senior scholar at the Johns Hopkins Center for Health Security. “They clearly are not getting to people at high enough rates to have their maximum impact.”
Currently, the federal government distributes four outpatient COVID treatments that can help stop the progression of COVID infections if taken within five to seven days of symptom onset, and one prevention therapy for immunocompromised people. State health departments and certain providers can order these drugs, and they are now available at pharmacies, infusion centers, and health clinics across the country.

But states and health care providers report that less than half of the supply of treatments that they’ve ordered starting October 2021 has been used.
Health experts initially expected the drugs to fly off the shelves. “I thought [utilization] would be much higher,” says Dr. Phyllis Tien, an infectious disease physician at University of California, San Francisco, who serves on the NIH COVID-19 treatment guidelines panel. At first, doctors were prioritizing who would get them, she says, to help preserve access for those with the greatest medical need.
The reported utilization rates may underestimate the total doses used; sites are supposed to report daily or weekly usage numbers to the government, but not all do. Still, the rates are used by the government to make decisions on distribution policies, and Tien says they track with what she’s seeing on the ground.
“When a patient comes to us and they’re COVID positive and they have some mild symptoms, we offer them some of these drugs if they fit the criteria,” she says, “But some of them don’t want to take the drugs. Others may want the drug, but they’re out of the window in terms of getting access to it.”
Unused drugs, at risk of being thrown out
The use rates vary by product, according to the data collected by HHS.
Two treatment options, recommended as alternative therapies only when other options are not available, have the lowest usage rates. Bebtelovimab is a monoclonal antibody injection authorized last month with “insufficient data” on key outcomes, according to NIH treatment guidelines; just 2{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} of the amount ordered by providers has been used, according to the HHS data.
The other with very low utilization is molnupiravir, a pill course typically recommended only when other, more effective options are not viable; just 14{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} of the doses sent out have been used.
Evusheld, a preventative shot of monoclonal antibodies that helps protect immunocompromised people from infection, is not widely used – just 54{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} of the 848,000 doses available have been sent out, and just a quarter of those ordered have been used.
Even the most highly recommended treatments are going unused. Hundreds of thousands of doses of sotrovimab are sitting in refrigerated storage — this monoclonal antibody infusion treatment is nearly 80{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} effective at preventing hospitalization from COVID for high-risk people. Likewise, hundreds of thousands of courses of Paxlovid, a highly effective pill that cuts the risk of getting hospitalized with COVID by nearly 90{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161}, are gathering dust on pharmacy shelves. For both these treatments, less than half of the distributed courses have been reported as used.
HHS’s Eisnor, speaking to health care providers in mid March, said he was troubled by reports that some pharmacies had asked if they could trash their remaining supplies of unexpired COVID pills. “We ask that you utilize any and all resources to facilitate [redirecting supply], maybe moving product outside to a neighboring state or jurisdiction or territory if they have a need,” he said.
What’s keeping people from using the drugs
These drugs are currently prioritized for people at high risk of COVID-19 (though sites and providers have discretion on who qualifies). Given the ready supply and low utilization rates, Tien says it may be time to expand the drug’s availability to people at lower risk who could still benefit from the drug.
“I had a situation last week where a young person who … got COVID called their physician for Paxlovid and was denied,” says Tien: The patient had a risk factor for COVID, but their doctor did not think they qualified for the drug, based on age and vaccination status. “There are some people who want it and are being turned away, and then there are others who perfectly fit the criteria and don’t want it,” Tien observes.
Health experts point to a litany of other factors that contribute to low COVID treatments utilization. “There is a lack of awareness from [patients and] providers,” says Adalja, “and challenges in understanding how to use them appropriately.” The COVID pills must be given within five days of symptom onset, and can be complicated to prescribe – for instance, Paxlovid can interfere with commonly taken medications and molnupiravir is not recommended for patients pregnant or trying to conceive.
Then, it can be hard to know which pharmacies have the pills in stock or which infusion clinics have appointments available. A patient needs to be able to quickly find a clinician, get a diagnosis and prescription, and be able to access the treatment, all within a few days.
“It’s multifactorial why these drugs are underutilized,” Adalja says, “It’s likely all of those things are playing some role in the discrepancies between what’s been ordered and and what’s actually been administered.”

The Biden administration launched the Test to Treat initiative this month to address these gaps. “We know the challenges that are involved with patients obtaining therapeutics,” said Dr. Meg Sullivan, acting chief medical officer for HHS’s Assistant Secretary for Preparedness and Response, in a call with clinicians on March 12. The program aims to improve access to rapid testing, and to bolster public and provider awareness of available COVID treatments and how to get them.
But the administration says their ability to support a continued pipeline of COVID drugs may soon be hindered by a lack of congressional funding. Senior administration officials told reporters March 15 that they may run out of monoclonal antibody treatments by May, and Evusheld by summer.
Since these therapies are currently only authorized for emergency use, they’re not available on the commercial market, so the government is the sole buyer, says Adalja. It also means they can’t be advertised by drug companies, which likely contributes to the lack of awareness of these treatments from providers and the public.
“It’s a bad situation when these drugs are going left unused, when we have people hospitalized and dying from COVID,” says Adalja. But he doesn’t find it surprising, given that lifesaving COVID vaccines are also expiring on pharmacy shelves and getting tossed every day. “It’s the way this pandemic has gone,” he says. “A lot of the medical countermeasures haven’t been able to be used optimally.”





More Stories
The Importance of Health and Wellness in Life
The Value of OmniChannel to Healthcare Providers
Unlocking Youthful Beauty: Exploring Veraclinic’s Expertise in Turkey Hair Transplant and Comprehensive Cosmetic Procedures