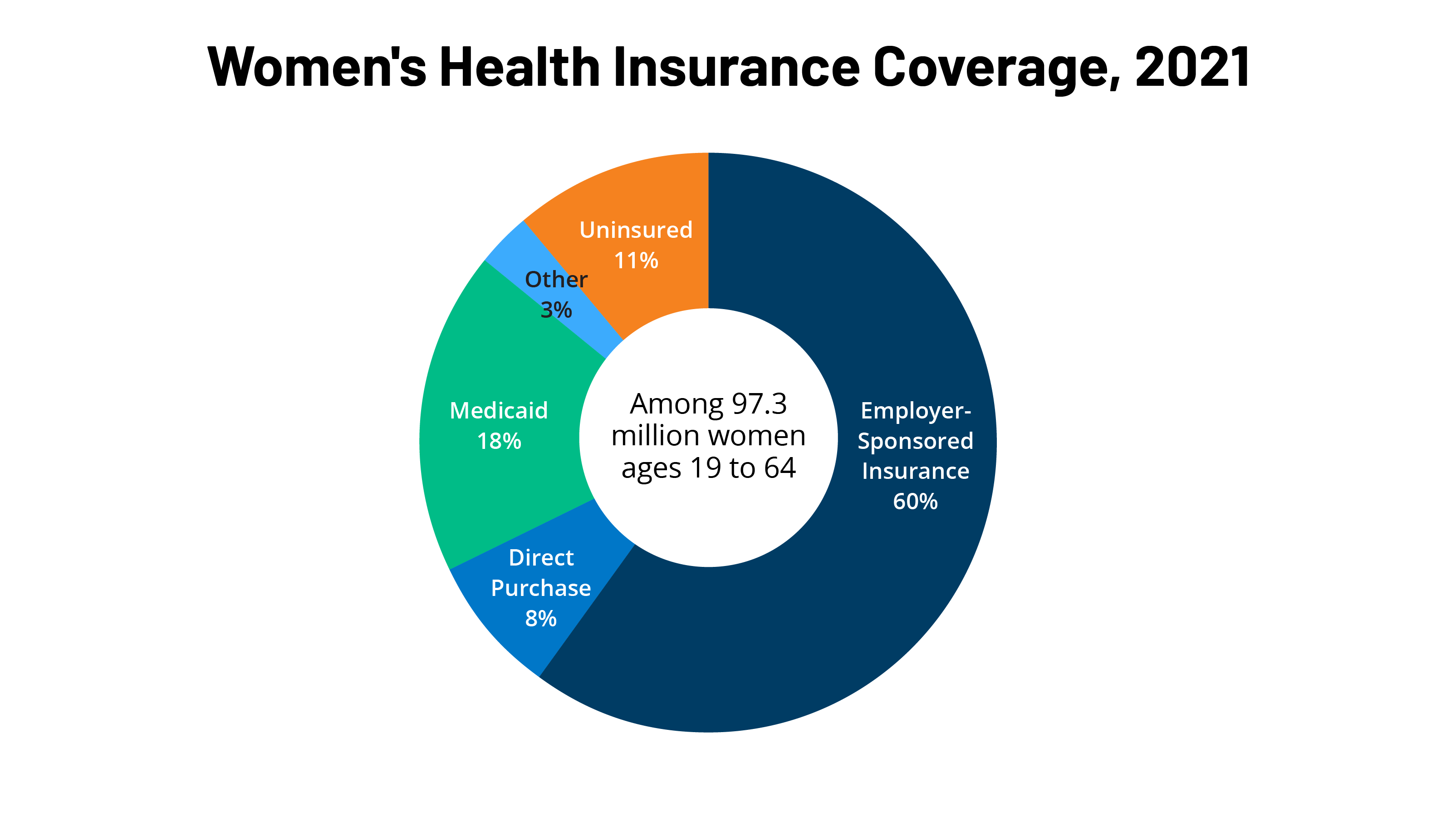
Health insurance coverage is an important factor in making health care affordable and accessible to women. Among the 97.3 million women ages 19 to 64 residing in the U.S., most had some form of coverage in 2021. However, gaps in private sector and publicly-funded programs and lack of affordability left a little over one in ten women uninsured. Over the past decade, the Affordable Care Act (ACA) has expanded access to affordable coverage through a combination of Medicaid expansions, private insurance reforms, and premium tax credits. This factsheet reviews major sources of coverage for women residing in the U.S. in 2021, as the coronavirus pandemic continued in the U.S. and globally, discusses the impact of the ACA on women’s coverage, and the coverage challenges that many women continue to face.
Sources of Health Insurance Coverage
Employer-Sponsored Insurance
Approximately 58.1 million women ages 19-64 (60{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161}) received their health coverage from employer-sponsored insurance in 2021 (Figure 1).
- Women in families with at least one full-time worker are more likely to have job-based coverage (71{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161}) than women in families with only part time workers (37{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161}) or without any workers (17{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161}).
- In 2021, annual insurance premiums for employer sponsored insurance averaged $7,739 for individuals and $22,221 for families. Family premiums have increased 47{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} over the last decade. On average, workers paid 17{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} of premiums for individual coverage and 28{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} for family coverage with the employers picking up the balance.
Non-Group Insurance
The ACA expanded access to the non-group or individually purchased insurance market by offering premium tax credits to help individuals purchase coverage in state-based health insurance Marketplaces. It also included many insurance reforms to alleviate some of the long-standing barriers to coverage in the non-group insurance market. In 2021, about 8{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} of women ages 19 to 64 (approximately 8.2 million women) and 8{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} of their male counterparts purchased insurance in the non-group market. This includes individuals who purchased private policies from the ACA Marketplace in their state, as well as those who purchased coverage from private insurers that operate outside of Marketplaces.
- Most individuals who seek insurance policies in their state’s Marketplace qualify for assistance with the costs of coverage. Individuals with incomes below $56,388 (400{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} of the Federal Poverty Level) can qualify for assistance in the form of federal tax credits which lower premium costs. The American Rescue Act (ARPA) of 2021, and subsequently the Inflation Reduction Act of 2022, provided a temporary extension (to 2025) of Marketplace subsidies to people with higher income levels.
- The ACA set new standards for all individually purchased plans, including plans available through the Marketplace as well as those that existed prior to the ACA. The ACA bars plans from charging women higher premiums than men for the same level of coverage (gender rating) or from disqualifying women from coverage because they had certain pre-existing medical conditions, including pregnancy. All direct purchase plans must also cover certain “essential health benefits” (EHBs) that fall under 10 different categories, including maternity and newborn care, mental health, and preventive care.
Medicaid
The state-federal program for low-income individuals, Medicaid, covered 18{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} of adult women ages 19 to 64 in 2021, compared to 14{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} of men. Historically, to qualify for Medicaid, women had to have very low incomes and be in one of Medicaid’s eligibility categories: pregnant, mothers of children 18 and younger, a person with a disability, or over 65. Women who didn’t fall into these categories typically were not eligible regardless of how poor they were. The ACA allowed states to broaden Medicaid eligibility to most individuals with incomes less than 138{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} of the FPL regardless of their family or disability status, effective January 2014. As of December 2022, 39 states and DC have expanded their Medicaid programs under the ACA—one state, South Dakota, has adopted but not yet implemented Medicaid expansion.
- Medicaid covers the poorest population of women. Forty-two percent of low-income women (income below 200{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} FPL) and 50{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} of poor women (income below 100{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} FPL) have Medicaid coverage.
- By federal law, all states must provide Medicaid coverage to pregnant women with incomes up to 133{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} of the federal poverty level (FPL) through 60 days postpartum. However, in recent years, there has been a growing interest in expanding the length of the postpartum coverage period, and to date, over half of states have taken steps to extend postpartum Medicaid coverage beyond 60 days. During the current COVID-19 public health emergency (PHE), states are providing continuous coverage to all Medicaid enrollees who have been enrolled in the program since March 18, 2020. Once the PHE is lifted and the continuous coverage ends though, postpartum women, particularly those living in states that have not taken up the ACA expansion or extended the postpartum period, are at risk of losing Medicaid coverage after 60 days.
- Medicaid financed 42{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} of births in the U.S. in 2020, accounts for 75{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} of all publicly-funded family planning services and half (52{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161}) of all long-term care spending, which is critical for many frail elderly women.
- Over half of the states (27 states) have established programs that use Medicaid funds to cover the costs of family planning services for low-income women who remain uninsured, and most states have limited scope Medicaid programs to pay for breast and cervical cancer treatment for certain low-income uninsured women.
- Under Medicaid, abortion coverage is very limited. The federal Hyde Amendment prohibits federal spending on abortions, except when the pregnancy is a result of rape or incest, or when it jeopardizes the life of the pregnant person. States may use their own unmatched funds to pay for abortions for Medicaid enrollees who see abortion in other circumstances. On June 24, 2022, the Supreme Court overturned Roe v. Wade, eliminating the federal Constitutional standard that had protected the right to abortion. Absent any federal standard addressing a right to abortion, states may set their own policies banning or protecting abortion. Many of the states that follow the Hyde restrictions now ban or are attempting to ban the provision of abortion.
Uninsured Women
Women are less likely than men to be uninsured, as a higher share of adult women are enrolled in Medicaid. On average, women have lower incomes and have been more likely to qualify for Medicaid than men under one of Medicaid’s eligibility categories; pregnant, parent of children under 18, disabled, or over 65. In 2021, 14{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} of men ages 19-64 were uninsured compared to approximately 11{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} of women in the same age bracket (10.3 million women). In spite of significant job losses, uninsured rates among women held steady during the second year of the COVID-19 pandemic, in part due to the continuous coverage requirements under Medicaid and the ongoing availability of subsidized coverage through the state-based health insurance exchanges.
Uninsured women often have inadequate access to care, get a lower standard of care when they are in the health system, and have poorer health outcomes. Compared to women with insurance, uninsured women have lower use of important preventive services such as mammograms, Pap tests, and timely blood pressure checks. They are also less likely to report having a regular doctor.
- Low-income women, women of color, and non-citizen women are at greater risk of being uninsured (Figure 2). One in five (19{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161}) women with incomes under 200{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} of the FPL ($28,194 for an individual in 2021) are uninsured (Table 2), compared to 7{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} of women with incomes at or above 200{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} FPL. Over one in five Hispanic (22{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161}) and American Indian and Alaska Native (22{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161}) women are uninsured. A higher share of single mothers are uninsured (11{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161}) than women in two-parent households (8{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161}).
- The majority of uninsured women live in a household where someone is working: 65{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} are in families with at least one adult working full-time and 79{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} are in families with at least one part-time or full-time worker.
- There is considerable state-level variation in uninsured rates across the nation, ranging from 23{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} of women in Texas to 3{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} of women in Washington DC, Massachusetts, and Vermont (Figure 3). Of the 17 states with uninsured rates above the national average (11{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161}), ten have not adopted the ACA Medicaid expansion.
- Many women who are uninsured are potentially eligible for financial assistance with coverage. Some are likely eligible for Medicaid but are not enrolled, while others qualify for subsidized Marketplace plans but may not be aware of coverage options or may face barriers to enrollment. However, in states that have not adopted the ACA Medicaid expansion, some poor uninsured women fall into a “coverage gap” because they earn too much to qualify for Medicaid but not enough to qualify for Marketplace premium tax credits. Other uninsured women are not eligible for any assistance with health coverage due to their immigration status, their income, or because they have an offer from an employer.
Scope of Coverage and Affordability
The ACA set national standards for the scope of benefits offered in private plans. In addition to the broad categories of essential health benefits (EHBs) offered by marketplace plans, all privately purchased plans must cover maternity care which had been historically excluded from most individually purchased plans. In addition, most private plans must cover preventive services without co-payments or other cost sharing. This includes screenings for breast and cervical cancers, well woman visits (including prenatal visits), prescribed contraceptives, breastfeeding supplies and supports such as breast pumps, and several STI services. There have been several legal challenges over elements of the preventive services policy, including in the currently pending case, Braidwood Management Inc. v. Becerra, which could affect whether the preventive services requirement remains intact in the future. Twenty-six states have laws banning coverage of most abortions from the plans available through the state Marketplaces. These restrictions were in place prior to the Supreme Court’s decision to overturn Roe v Wade.
Affordability of coverage continues to be a significant concern for many women, both for those who are uninsured as well as those with coverage. The leading reason why uninsured adults report that they haven’t obtained coverage is that it is too expensive. Under employer-sponsored insurance, the major source of coverage for women, 61{6f90f2fe98827f97fd05e0011472e53c8890931f9d0d5714295052b72b9b5161} of all covered workers with a general annual deductible have deductibles of at least $1,000 for single coverage. Thirty-seven percent of women with employer sponsored coverage report that it is difficult to meet their deductibles.
Looking Forward
Health coverage matters for women. Those with health coverage are more likely to obtain needed preventive, primary, and specialty care services, and have better access to new advances in women’s health. Today, because of the ACA, most women can get coverage without worrying that they will be charged more for insurance than men, have insurance that provides them with no-cost coverage for a wide range of recommended preventive services, and coverage for critical services for women such as maternity care. The uninsured rate has declined significantly over the past decade; however, 10 million women remain uninsured, with rates highest in states that have not expanded Medicaid eligibility.





More Stories
Exploring the Magic of Sapphire Engagement Rings in Birmingham’s Jewelry Quarter
Unlocking the Expertise of Women’s Care Specialists: A Comprehensive Guide
Women’s Birth and Wellness Center: A Comprehensive Guide